Annual Physical (Non-Medicare) Extra Charge Trickery
Today we report on an annoying trend we’ve seen clients experience more frequently of late. In fact, two of us at Healthcare Navigation have been subjected to overbilling in this manner. The overbilling occurs when a second visit charge is added to the annual physical exam without justification. Such a charge can be legitimate but often it is not. You’ll recall that the Affordable Care Act changes of 2014 required ACA-compliant plans to include the physical exam as a benefit paid for through the premium. That means charges for the annual physical should not be applied to the deductible and there should be no coinsurance or copayment for those services.
If at your physical appointment you present a distinct problem you’d like the doctor to see like a rash or a wound that isn’t healing, that is a legitimate second visit charge because it is not well care which is how the physical exam would be coded. However, more patients are charged for an additional visit when it doesn’t appear to be legitimate.
When this happened to me, I was impressed with how well-trained the billing staff were in explaining how a second visit charge occurs. But I pushed back and asked the staff to review the medical record and tell me what the second visit charge was related to. They ended up writing that charge off. It wasn’t a great deal of money but it was not a legitimate charge.
Another colleague didn’t fare as well. She was charged $219 for a second visit charge (see physician statement below).
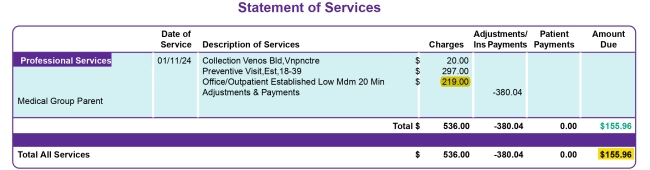
When she called the office to inquire, the office staff reported that the physician’s notes indicated that in response to a question about how she was doing, she had responded that she was feeling tired that day. Working women who are also mothers of young children often do report fatigue but really? That was a casual conversation, not a complaint that required medical intervention.
We have sympathy with physicians and other providers dealing with low in-network payment rates but we also feel that imagination should not play a role in what services are submitted as claims to an insurer and then billed to the patient. It may be small scale insurance fraud but in those instances when a second visit is tacked on without any clinical justification, that is insurance fraud.
Again, it is wise to get in the habit of carefully reviewing your medical bills at a detailed level. That skill often pays dividends if you take the time to challenge what doesn’t seem right.




