An Interesting but Underwhelming Generic Drug Journey
There has been quite a bit of publicity lately related to Mark Cuban’s Cost Plus Drug Program and Amazon Prime launching their drug distribution services. Today’s video addresses this topic. Affording prescription drugs is a serious problem for many Americans but my limited exercise suggests that many generics are indeed fairly inexpensive. Unfortunately, there isn’t apparent relief where it truly hurts, i.e., prescription drugs for which there is no generic version available.
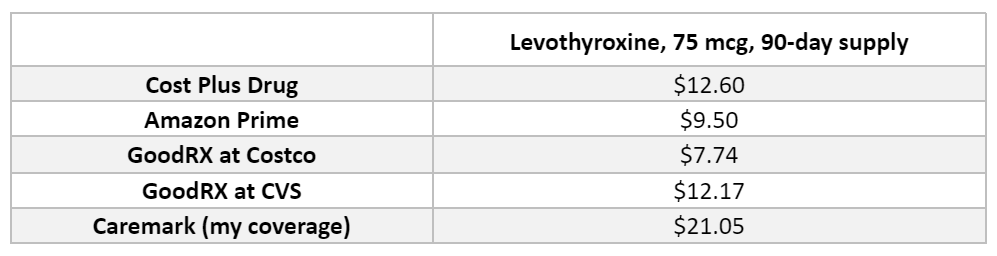
Although I picked a low- cost drug, I found that the most expensive way to fill it was through my insurance which is, no doubt, maddening. After all, filling a prescription outside my insurance results in the cost not being applied to my prescription deductible. At the same time, as you can see from the below table, the costs are low.
I looked at the cost of Levothyroxine and its associated brand, Synthroid. A breakdown for Levothyroxine is below. When a program only had data for a 30-day supply, that figure was multiplied by three for consistency. The cost of Synthroid across all researched vendors was steadily in the range of $140 to $150 for a 90-day supply. As mentioned in the video, I last paid $36.62 for a 90-day supply which was because I had met my deductible in late 2022 and my Plan was covering the balance of the cost. It is likely that the total cost of the drug was also in the $140- to $150-range we saw across the other suppliers.
I ended up filling my prescription with Amazon Prime because the site asked me for insurance information so I thought my order might be processed through insurance. The service was very efficient. My doctor was contacted for a new prescription, I received a 30-day supply quickly and was only charged $3.80. But no claim information was submitted according to my Caremark site. But for the $3.80 that would have been applied to my deductible, anyway, I am not concerned, just curious.
For low-cost generics, using these programs can be a cost saver, especially if you are in a high-deductible plan. If you are someone who believes you will easily meet your deductible or out-of-pocket maximum, however, it probably does not make sense to use these programs. But, if you have a high deductible and only fill a handful of inexpensive generics, these programs may be a good option. At the same time, if you are prescribed a drug that’s more expensive later in the benefit year which leads you to return to filling prescriptions through your drug coverage, you may have a touch of buyer’s remorse that the prescriptions you filled outside of your coverage cannot be applied to your deductible. You can’t know so choose the option with which you’re most comfortable.
We are hopeful these “disrupters” one day have an impact on bringing down the costs of drugs that are unaffordable. According to the press reports, they have big plans. We’ll see.




